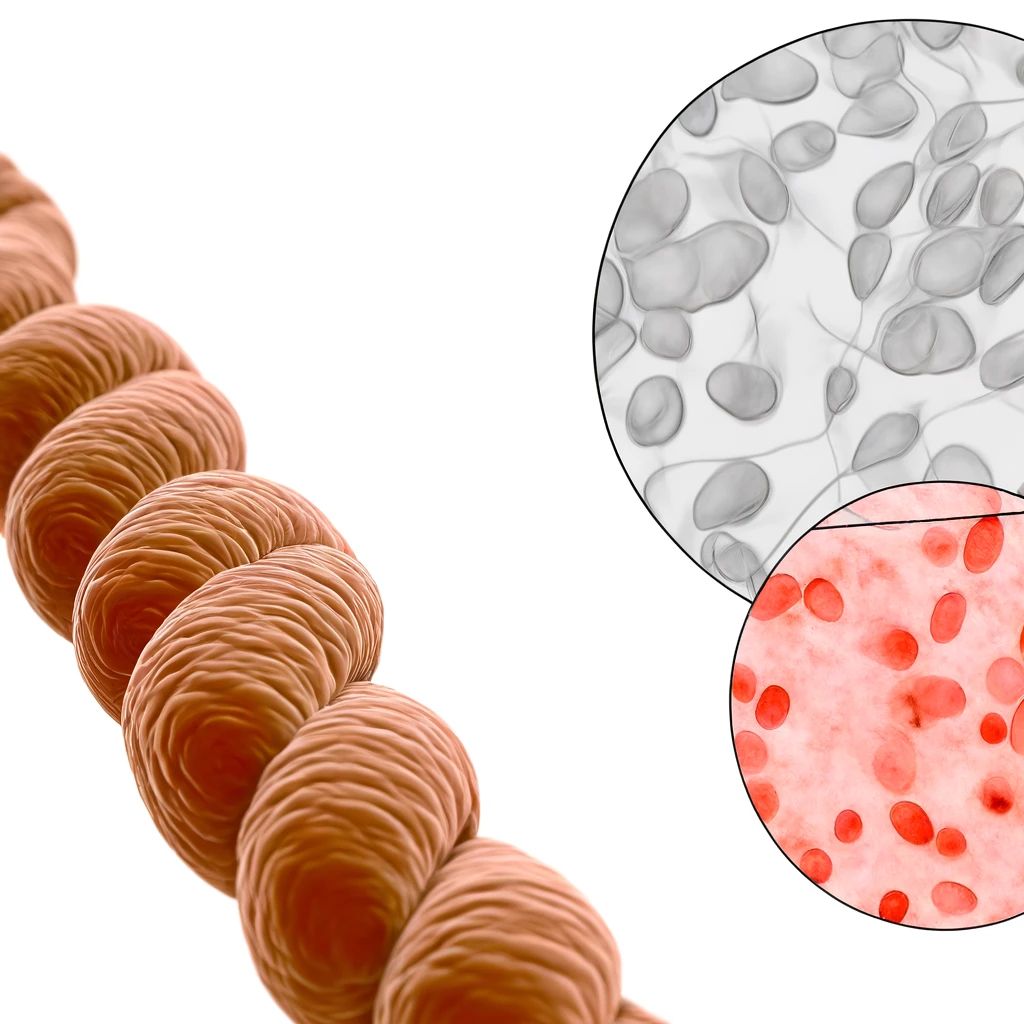
In the field of regenerative medicine, the choice between umbilical mesenchymal stem cells (UMSCs) and autologous (self-derived) mesenchymal stem cells (MSCs) is crucial. Here, we delve into the reasons why UMSCs are often the preferred option, supported by recent studies.
Availability and Abundance
Umbilical mesenchymal stem cells (UMSCs) are harvested from the umbilical cords, which are typically discarded after childbirth. This provides an abundant and ethically uncontroversial source of stem cells. The process of collecting UMSCs is straightforward and non-invasive, involving the collection of umbilical cord tissue postpartum, posing no risk to either the mother or the newborn. This contrasts with the harvesting of autologous MSCs, which necessitates invasive procedures like bone marrow aspiration or liposuction to obtain cells from the patient’s own body. These procedures can be painful, carry risks of complications, and often result in a limited yield of stem cells. The ease of access and ethical considerations surrounding UMSCs make them a highly attractive source for regenerative therapies.
Reference Study: Wang, S., et al. (2018). “Umbilical Cord-Derived Mesenchymal Stem Cells for Treating Myocardial Infarction: In Vitro and In Vivo Evaluation”. Stem Cell Research & Therapy, 9:29.
Proliferative Capacity
One of the key advantages of UMSCs is their superior proliferative capacity compared to autologous MSCs, particularly those derived from older individuals. UMSCs have a high ability to expand in culture, meaning that even a small initial sample can yield a large number of cells for therapeutic use. This is crucial in clinical applications where a high dose of cells is often required. In contrast, MSCs from older donors or patients with chronic diseases may have reduced proliferative ability, limiting their effectiveness. Studies have shown that UMSCs retain their proliferative and differentiation potential better than MSCs from adult tissues, making them a more reliable source for regenerative medicine.
Reference Study: Wang, S., et al. (2018). “Umbilical Cord-Derived Mesenchymal Stem Cells for Treating Myocardial Infarction: In Vitro and In Vivo Evaluation”. Stem Cell Research & Therapy, 9:29.
Immunomodulatory Properties
UMSCs possess strong immunomodulatory properties, which are beneficial in treating a range of inflammatory and autoimmune diseases. They have been shown to modulate the immune response by secreting various cytokines and growth factors that can suppress inflammation and promote tissue repair. Importantly, UMSCs express lower levels of major histocompatibility complex (MHC) antigens compared to autologous MSCs. This reduces the likelihood of immune rejection when UMSCs are transplanted into a patient, making them suitable for allogeneic (donor-derived) transplantation. The ability of UMSCs to evade the immune system and their robust immunomodulatory effects make them highly effective in clinical applications.
Reference Study: Le Blanc, K., & Davies, L. C. (2018). “Mesenchymal Stromal Cells and the Innate Immune Response”. Immunology Letters, 168(2): 140-146.
Reduced Senescence
Senescence, the process by which cells age and lose their ability to divide and function, is a significant concern in regenerative medicine. UMSCs are derived from neonatal tissues and have undergone fewer cellular divisions compared to MSCs from adult donors. This means they exhibit lower levels of cellular senescence and retain their functional potency for longer periods. In contrast, autologous MSCs, especially from older individuals, often show signs of senescence, reducing their effectiveness in regenerative therapies. The youthful nature of UMSCs contributes to their high therapeutic potential, as they are more likely to maintain their regenerative capabilities over time.
Reference Study: Kern, S., et al. (2006). “Comparative Analysis of Mesenchymal Stem Cells from Bone Marrow, Umbilical Cord Blood, or Adipose Tissue”. Stem Cells, 24(5): 1294-1301.
Ethical and Practical Considerations
The collection of UMSCs is non-invasive and poses no risk to the donor or the mother, making it an ethically sound practice. The umbilical cord, once considered medical waste, is now recognized as a valuable source of stem cells. This method of collection avoids the ethical and practical challenges associated with obtaining autologous MSCs, which require invasive procedures. For patients, this means access to a safer, pain-free source of stem cells. The ethical appeal and practical advantages of UMSCs enhance their desirability for both patients and clinicians.
Reference Study: Troyer, D. L., & Weiss, M. L. (2008). “Concise Review: Wharton’s Jelly-Derived Cells Are a Primitive Stromal Cell Population”. Stem Cells, 26(3): 591-599.
Consistency and Quality Control
One of the significant advantages of UMSCs is their ability to be banked and standardized. Cord blood banks can store UMSCs under controlled conditions, ensuring consistent quality and potency across different batches. This standardization is critical for clinical applications, where variability in cell quality can affect treatment outcomes. In contrast, autologous MSCs can vary significantly in quality and quantity due to individual differences in health, age, and environmental factors. The ability to produce a consistent and high-quality product makes UMSCs a more reliable choice for regenerative therapies.
Reference Study: Bieback, K., et al. (2008). “Critical Parameters for the Isolation of Mesenchymal Stem Cells from Umbilical Cord Blood”. Stem Cells, 26(3): 696-706.
Conclusion
The advantages of umbilical mesenchymal stem cells (UMSCs) over autologous MSCs are compelling. From their superior availability and proliferative capacity to their robust immunomodulatory properties and lower risk of senescence, UMSCs provide a versatile and potent option for various therapeutic applications. Their non-invasive collection process and ability to be standardized further solidify their status as the preferred choice in regenerative medicine.
For more detailed discussions and the latest updates on stem cell therapy, stay tuned to our blog.
References:
- Wang, S., et al. (2018). “Umbilical Cord-Derived Mesenchymal Stem Cells for Treating Myocardial Infarction: In Vitro and In Vivo Evaluation”. Stem Cell Research & Therapy, 9:29.
- Le Blanc, K., & Davies, L. C. (2018). “Mesenchymal Stromal Cells and the Innate Immune Response”. Immunology Letters, 168(2): 140-146.
- Kern, S., et al. (2006). “Comparative Analysis of Mesenchymal Stem Cells from Bone Marrow, Umbilical Cord Blood, or Adipose Tissue”. Stem Cells, 24(5): 1294-1301.
- Troyer, D. L., & Weiss, M. L. (2008). “Concise Review: Wharton’s Jelly-Derived Cells Are a Primitive Stromal Cell Population”. Stem Cells, 26(3): 591-599.
- Bieback, K., et al. (2008). “Critical Parameters for the Isolation of Mesenchymal Stem Cells from Umbilical Cord Blood”. Stem Cells, 26(3): 696-706.