Understanding Diabetic Retinopathy
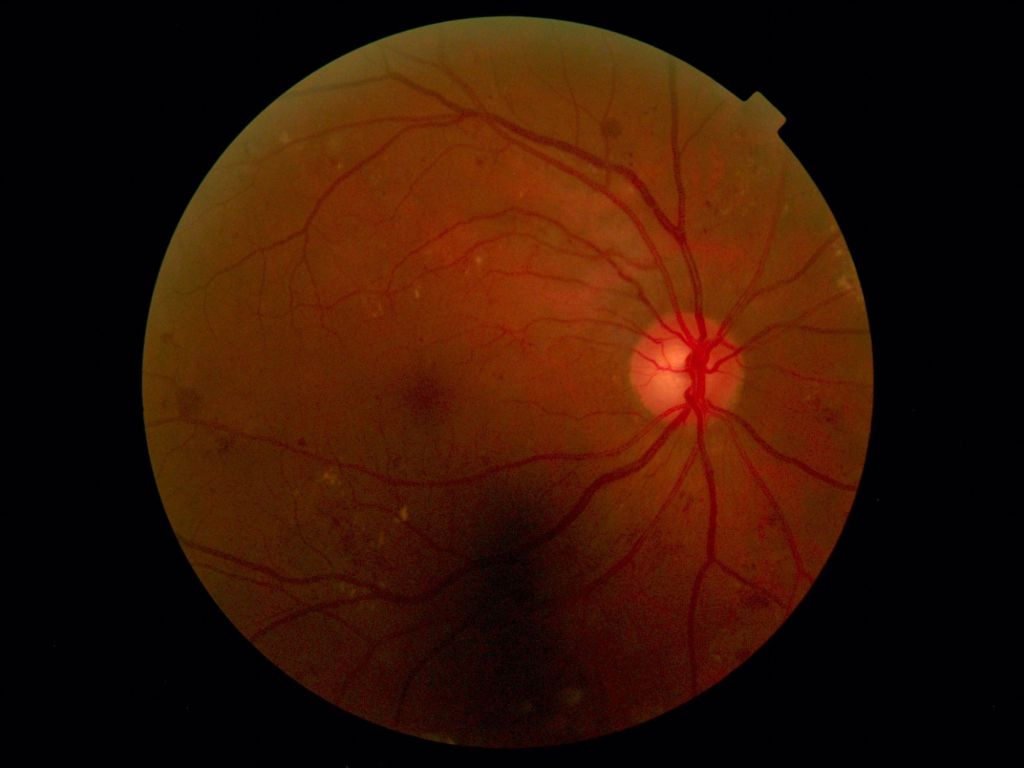
Diabetic retinopathy is a common complication of diabetes that affects the eyes. It occurs when high blood sugar levels cause damage to the blood vessels in the retina, potentially leading to vision loss if untreated. The condition progresses through several stages, starting from mild nonproliferative retinopathy to proliferative diabetic retinopathy (PDR), where new abnormal blood vessels begin to grow on the surface of the retina. If not managed properly, diabetic retinopathy can lead to severe vision impairment or even blindness.
The retina is a thin layer of tissue at the back of the eye that converts light into neural signals, which are then sent to the brain for visual recognition. When the retinal blood vessels are damaged due to high blood sugar levels, they can swell, leak, or become blocked. In advanced stages, new, abnormal blood vessels grow, which are fragile and prone to bleeding, leading to further vision problems.

Current Treatment Options
Traditional treatments for diabetic retinopathy focus on managing the underlying diabetes and preventing further progression of the eye disease. These treatments include:
- Blood Sugar Control: Keeping blood sugar levels within a target range through diet, exercise, and medications is crucial in preventing the onset and progression of diabetic retinopathy.
- Blood Pressure and Cholesterol Management: Controlling blood pressure and cholesterol levels helps reduce the risk of vascular complications in the retina.
- Laser Surgery: Laser photocoagulation is used to seal or shrink abnormal blood vessels and prevent them from leaking. This treatment can help slow or stop the progression of the disease but often does not restore lost vision.
- Vitrectomy: This surgical procedure involves removing the vitreous gel from the eye and replacing it with a saline solution. It is used to treat severe bleeding or retinal detachment in advanced diabetic retinopathy.
- Anti-VEGF Injections: Medications that block vascular endothelial growth factor (VEGF) are injected into the eye to reduce the growth of abnormal blood vessels and decrease fluid leakage. These injections can improve vision and prevent further damage.
While these treatments can be effective in managing the disease, they often come with significant side effects and may not completely halt the progression of diabetic retinopathy. Additionally, they do not address the underlying damage to the retinal tissues.
MSC Therapy: A Promising Solution
Mesenchymal Stem Cell (MSC) therapy is emerging as a promising treatment option for diabetic retinopathy. MSCs are multipotent stem cells found in various tissues, including bone marrow, adipose tissue, and umbilical cord blood. They have the potential to differentiate into a variety of cell types, including bone, cartilage, and fat cells. More importantly, MSCs possess immunomodulatory, anti-inflammatory, and regenerative properties, making them a valuable tool in treating various degenerative diseases, including diabetic retinopathy.
Mechanisms of Action
MSCs contribute to tissue repair and regeneration through several mechanisms:
- Anti-inflammatory Effects: MSCs secrete cytokines and growth factors that modulate the immune response and reduce inflammation, which is a key factor in the progression of diabetic retinopathy. Inflammation plays a crucial role in the damage to retinal blood vessels and the progression of the disease.
- Angiogenesis: MSCs promote the formation of new blood vessels, which can help repair the damaged retinal vasculature. This process, known as angiogenesis, is vital for restoring proper blood flow and oxygen supply to the retina.
- Neuroprotection: MSCs release neurotrophic factors that protect retinal neurons from apoptosis (programmed cell death) and support their survival. Neuroprotection is essential in preventing the loss of retinal neurons and preserving vision.
- Paracrine Signaling: MSCs exert their therapeutic effects mainly through the secretion of bioactive molecules that promote cell survival, reduce fibrosis, and enhance angiogenesis. These molecules, known as paracrine factors, play a critical role in mediating the beneficial effects of MSC therapy.
Key Studies Supporting MSC Therapy in Diabetic Retinopathy
- Li, J., Zhang, J., Zhang, Y., Tang, W., & He, Y. (2019). Mesenchymal Stem Cells Ameliorate Diabetic Retinopathy by Inhibiting Inflammation and Improving Retinal Vascular Function. Journal of Translational Medicine, 17(1), 1-11.
- Summary: This study demonstrated that MSC therapy significantly reduced retinal inflammation and improved vascular function in diabetic rats, suggesting a protective effect against diabetic retinopathy. The researchers found that MSCs modulate the inflammatory environment in the retina and enhance blood-retinal barrier integrity.
- Gomez-Montalvo, J. A., Garcia-Garcia, E., Esquivel-Garcia, E. S., Esquivel-Garcia, E., & Gonzalez-Gonzalez, J. G. (2020). Intravitreal Injection of Mesenchymal Stem Cells Reduces Retinal Degeneration and Vascular Leakage in a Mouse Model of Diabetic Retinopathy. Stem Cell Research & Therapy, 11(1), 1-12.
- Summary: Intravitreal injection of MSCs was found to decrease retinal degeneration and vascular leakage, highlighting the potential of MSCs in preserving retinal health in diabetic patients. The study provided evidence that MSCs can migrate to the damaged retinal areas and exert protective effects through their paracrine actions.
- Xiao, Y., Yang, J., Wu, Q., Xu, J., Wang, W., & Li, Y. (2021). Human Umbilical Cord-Derived MSCs for Treating Diabetic Retinopathy: A Preclinical Study. Investigative Ophthalmology & Visual Science, 62(8), 24.
- Summary: This preclinical study showed that human umbilical cord-derived MSCs could effectively reduce retinal neovascularization and improve visual function in diabetic models. The researchers highlighted the safety and efficacy of umbilical cord-derived MSCs in treating retinal vascular diseases.
- Wang, Q., Dong, Y., Luo, X., Zhang, Z., & Wang, J. (2022). Systemic Administration of MSCs Ameliorates Diabetic Retinopathy by Modulating Immune Response and Enhancing Retinal Cell Survival. Molecular Vision, 28, 273-285.
- Summary: Systemic administration of MSCs was shown to modulate immune responses and enhance the survival of retinal cells, offering a potential therapeutic avenue for diabetic retinopathy. The study suggested that MSCs could provide long-lasting benefits by altering the systemic inflammatory state and promoting retinal repair.
Conclusion
MSC therapy holds great promise for the treatment of diabetic retinopathy, offering hope for preserving vision and improving the quality of life for diabetic patients. The ability of MSCs to modulate the immune environment, promote vascular repair, and protect retinal neurons makes them a versatile and powerful therapeutic tool. As research progresses, we anticipate even more breakthroughs in this exciting field, potentially revolutionizing the management of diabetic retinopathy and other retinal diseases.
Stay Informed
Follow our page for the latest updates on stem cell therapies and other innovative treatments for diabetic complications. We are committed to providing the most current and comprehensive information to help improve patient outcomes and advance the field of regenerative medicine.