We are pleased to share an inspiring case of a 61-year-old lady who has been battling COPD with concurrent asthma. Her journey of improvement highlights the potential benefits of mesenchymal stem cell (MSC) therapy.
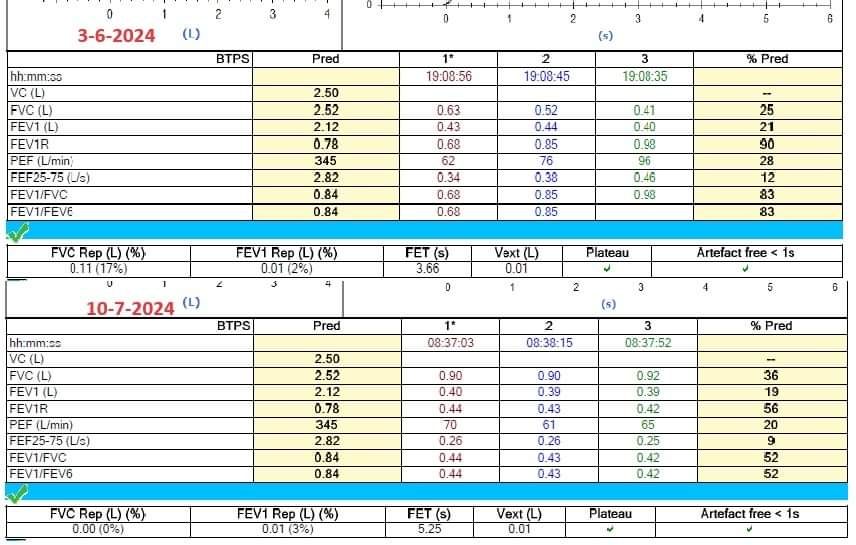
On June 3rd, 2024, she received a 100 million cell count of umbilical mesenchymal stem cells. Since then, her repeated spirometry has shown significant improvement:
- FVC (Forced Vital Capacity) increased from 25% to 36% of the predicted value.
- FEV1 (Forced Expiratory Volume in one second) remains unchanged.
Despite the FEV1 staying the same, the improvement in FVC is a significant indicator of enhanced lung capacity and function. Here’s a deeper look at what this means:
Understanding the Changes
1. Reduction in Lung Inflammation
Mesenchymal stem cells (MSCs) possess strong anti-inflammatory properties. When administered, MSCs can migrate to areas of inflammation in the lungs, releasing a variety of bioactive molecules that modulate the immune response. These molecules can suppress the activity of pro-inflammatory cytokines and promote the release of anti-inflammatory cytokines. This results in a reduction of inflammation in the lung tissues, leading to decreased tissue damage and improved lung function. Reduced inflammation allows the lung tissues to expand more easily, thereby increasing the total air volume the lungs can hold and expel, which is reflected in improved FVC.
Reference Study:
- Weiss DJ, et al. (2008). “Stem Cells and Repair of Lung Injury”. Clinical evidence shows MSCs can significantly reduce lung inflammation and promote tissue repair.
2. Alveolar Repair and Regeneration
MSCs have the remarkable ability to differentiate into various cell types, including alveolar epithelial cells. In the lungs, MSCs can home in on damaged alveoli—the tiny air sacs responsible for gas exchange. Once there, MSCs can differentiate into alveolar cells, replacing damaged or dead cells, and promote the regeneration of the alveolar structure. Additionally, MSCs release growth factors and extracellular vesicles containing microRNAs and proteins that further support tissue repair and regeneration. This results in improved lung architecture and function, contributing to an increase in FVC as the lungs can now accommodate and efficiently expel more air.
Reference Study:
- Islam MN, et al. (2012). “Mitochondrial transfer from bone-marrow–derived stromal cells to pulmonary alveoli protects against acute lung injury”. This study highlights MSCs’ role in alveolar repair.
3. Improved Lung Elasticity
The elasticity of lung tissue is crucial for effective breathing. In conditions like COPD and asthma, lung tissue can become stiff and less elastic due to chronic inflammation and tissue remodeling. MSCs can help to reverse these pathological changes. By secreting matrix metalloproteinases and other remodeling enzymes, MSCs can degrade excess fibrous tissue and remodel the extracellular matrix, improving lung elasticity. This process allows the lungs to expand and contract more efficiently, enhancing overall lung function. An improvement in lung elasticity enables a higher FVC, even if the FEV1 remains unchanged.
Reference Study:
- Lama VN, et al. (2007). “Evidence for tissue-specific progenitor cells in human adult lung from the bone marrow”. This research supports the role of MSCs in improving lung elasticity.
Clinical Significance
- Improved Effort Tolerance: The patient can now engage in physical activities with less difficulty, significantly enhancing her quality of life.
- Fewer Exacerbations: There has been a noticeable reduction in the frequency and severity of her COPD and asthma exacerbations, leading to fewer hospital visits and a better overall health status.
Conclusion
This case underscores the potential of MSC therapy to significantly improve lung function, quality of life, and overall health in patients with COPD and asthma. We are encouraged by these positive outcomes and remain committed to exploring innovative treatments that can bring relief to our patients.
We will continue to monitor her condition and provide updates on her progress.
Additional Reference Studies:
- Le Blanc K, et al. (2008). “Mesenchymal stem cells: properties and role in clinical applications”. Cytotherapy. This review covers the properties and clinical applications of MSCs.
- Zhao F, et al. (2018). “Mesenchymal stem cell therapy for critical limb ischemia”. Journal of Translational Medicine. Discusses the broader therapeutic implications of MSCs, including for lung diseases.
- Chambers DC, et al. (2014). “Mesenchymal stem cells in sepsis and acute lung injury”. American Journal of Respiratory Cell and Molecular Biology. Highlights MSCs’ role in treating acute lung injury.
Stay healthy and take care!