Introduction
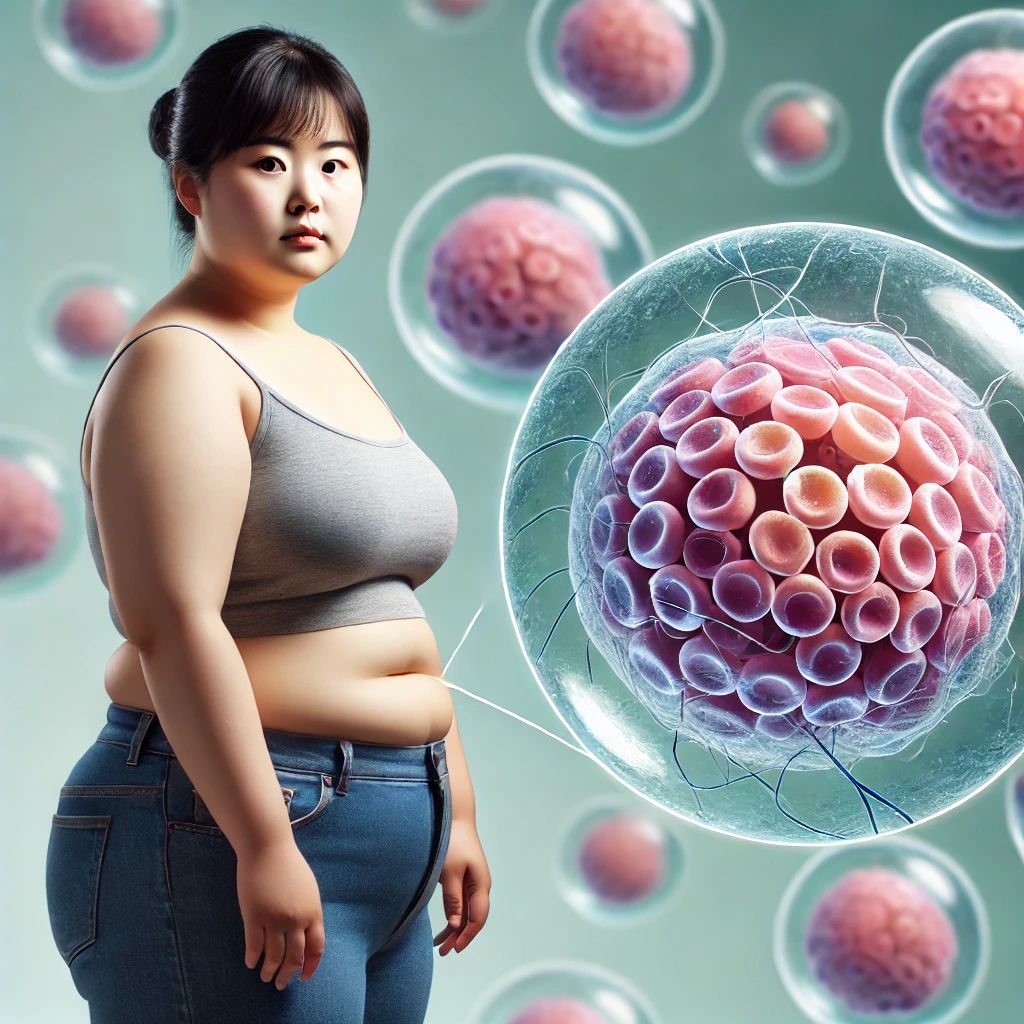
Obesity is a significant global health concern, characterized by excessive fat accumulation that presents a risk to health. This chronic and multifactorial condition is linked to numerous health issues, including type 2 diabetes, cardiovascular diseases, and certain cancers. Traditional treatments, such as diet, exercise, and medications, often struggle to provide sustainable long-term results. However, recent advancements in Mesenchymal Stem Cell (MSC) therapy have shown promising potential in treating obesity and its related metabolic disorders.
Understanding Mesenchymal Stem Cells (MSCs)
MSCs are multipotent stromal cells that can differentiate into various cell types, including adipocytes, chondrocytes, and osteoblasts. They can be derived from multiple sources, such as bone marrow, adipose tissue, and Wharton’s jelly. MSCs possess unique immunomodulatory and regenerative properties, making them an attractive option for treating various conditions, including obesity.
Therapeutic Effects of MSCs in Metabolic Syndrome
One significant study by Gupta et al. (2020) explored the therapeutic effects of Wharton’s jelly-derived MSCs in a rat model of metabolic syndrome. The research demonstrated that a single high-dose intravenous injection of these MSCs led to significant improvements in metabolic profiles and reduced inflammation. Specifically, the treatment resulted in better regulation of blood glucose levels, improved lipid profiles, and decreased systemic inflammation. These findings suggest that MSCs could be effective in addressing the underlying metabolic dysfunctions and inflammatory processes that contribute to obesity-related conditions.
Adipose-Derived MSCs (ADMSCs) and Gene Therapy
Another promising avenue is the use of adipose-derived MSCs (ADMSCs). Saleh et al. (2023) highlighted the potential of gene therapy using ADMSCs to improve metabolic health, reduce inflammation, and support tissue regeneration. By genetically modifying ADMSCs, researchers can enhance their therapeutic potential, ensuring better survival and functionality in the damaged tissue environments typical of obesity. These modified cells can secrete various bioactive molecules, such as growth factors and adipokines, crucial for modulating metabolic pathways and improving overall metabolic health.
Systematic Review of ADMSCs
A systematic review conducted by Saleh et al. (2023) collated evidence from several preclinical studies on ADMSCs. The review demonstrated consistent positive outcomes in body weight, glucose metabolism, lipid profiles, and systemic inflammation in animal models. This strong preclinical evidence suggests that ADMSCs could be a viable option for obesity treatment, potentially leading to clinical trials to further validate these findings.
Antioxidant-Upregulated MSCs
In another innovative approach, Fathi-Kazerooni et al. (2020) explored the use of antioxidant-upregulated MSCs in a diet-induced obesity model. The study showed that these modified MSCs effectively reduced body weight gain and improved overall metabolic health. The enhanced MSCs could better survive oxidative stress and maintain their therapeutic efficacy in inflamed and metabolically dysregulated environments. This method could significantly enhance the effectiveness of MSC therapy by protecting the cells from the hostile conditions present in obese patients.
Preventing Weight Gain and Hyperglycemia
Research by Saleh et al. (2020) demonstrated that ADMSCs could prevent body weight gain and hyperglycemia in obese mice. The study found that the injection of ADMSCs led to significant reductions in body weight and improved glucose tolerance. These results highlight the potential of ADMSCs to modulate adipose tissue function and improve insulin sensitivity, making them a promising therapeutic option for managing obesity and its associated metabolic disorders.
Conclusion
The studies discussed above collectively suggest that MSC therapy holds great promise for addressing obesity and its complications. By leveraging the unique properties of MSCs, particularly those derived from adipose tissue and Wharton’s jelly, researchers can develop novel and potentially effective treatment strategies for obesity. These therapies target the underlying metabolic dysfunctions and inflammatory processes, offering a new hope for sustainable and long-term obesity management.
References
- Gupta N, Su X, Popov B, et al. (2020). Single high-dose intravenous injection of Wharton’s jelly-derived mesenchymal stem cell exerts protective effects in a rat model of metabolic syndrome. Stem Cell Research & Therapy, 11, 177.
- Saleh F, Itani L, Calugi S, Dalle Grave R, El Ghoch M. (2023). Gene Therapy Based on Mesenchymal Stem Cells Derived from Adipose Tissue for the Treatment of Obesity and Its Metabolic Complications. International Journal of Molecular Sciences, 24(8), 7468.
- Saleh F, Itani L, Calugi S, Dalle Grave R, El Ghoch M. (2023). Adipose-derived Mesenchymal Stem Cells in the Treatment of Obesity: A Systematic Review of Longitudinal Studies on Preclinical Evidence. Stem Cell Research & Therapy, 14, 215.
- Fathi-Kazerooni M, Fattah-Ghazi S, Darzi M, et al. (2020). Antioxidant-upregulated mesenchymal stem cells reduce inflammation and improve fatty liver disease in diet-induced obesity. Stem Cell Research & Therapy, 11, 217.
- Saleh F, Itani L, Calugi S, Dalle Grave R, El Ghoch M. (2020). Adipose-derived mesenchymal stem cells from obese mice prevent body weight gain and hyperglycemia. Stem Cell Research & Therapy, 11, 789.
By continuing to explore and validate these innovative MSC-based therapies, we can move closer to finding effective and sustainable solutions for obesity and its associated health risks. Stay tuned for more updates on cutting-edge treatments and health tips!