A 37-year-old male with diabetes, on standard medication, recently received mesenchymal stem cell (MSC) therapy as an adjunct treatment. His recent blood tests reveal important insights into his metabolic state and the potential role of regenerative therapy in chronic disease management.
Latest Diabetic Panel Results
- Fasting Glucose: 3.6 mmol/L (Normal, low side)
- HbA1c: 7.2% (Above recommended target; optimal control <6.5–7.0%)
- Insulin: 3.1 µIU/mL
- C-Peptide: 1.29 ng/mL (Both insulin and C-peptide are low-normal)
- HOMA-IR (Insulin Resistance Index): 0.5 (Indicates minimal insulin resistance)

Interpretation of the Results
Despite having a normal fasting glucose, the patient’s HbA1c is elevated, indicating that his average blood sugar over the past three months has been above optimal. His low-normal insulin and C-peptide levels point toward reduced pancreatic insulin secretion. The HOMA-IR score is low, suggesting that insulin resistance is not the primary issue.
Conclusion: The patient’s diabetes appears to be due primarily to inadequate insulin production rather than insulin resistance, which is common in early-onset or long-standing type 2 diabetes, or in cases with pancreatic beta-cell exhaustion.
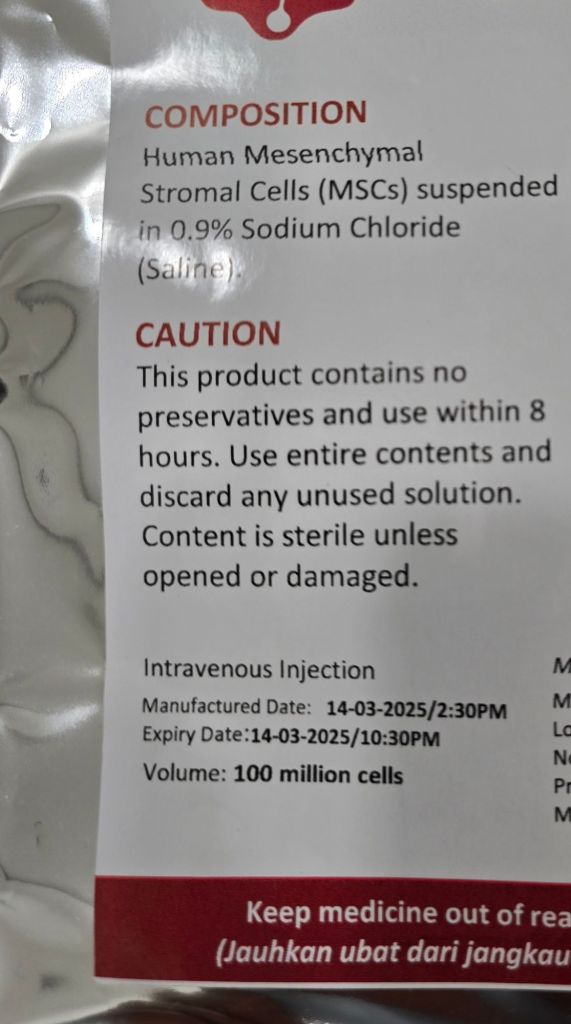
How Mesenchymal Stem Cell (MSC) Therapy May Help
MSC therapy is an emerging field with promising results in diabetes management, especially in cases with declining insulin production. The therapy utilizes the regenerative and immunomodulatory capabilities of MSCs to potentially improve pancreatic function and overall metabolic health.
Key Benefits of MSC Therapy in Diabetes:
- Beta-Cell Regeneration and Protection
MSCs secrete a range of growth factors and cytokines that promote regeneration of pancreatic beta cells and protect existing ones from damage. - Immunomodulatory and Anti-Inflammatory Effects
MSCs help reduce systemic and pancreatic inflammation, calming autoimmune activity and improving the internal environment for beta-cell survival and function. - Improved Glycemic Control
Clinical studies have shown MSC therapy can lower HbA1c levels, improve insulin sensitivity, and reduce the need for external insulin or oral hypoglycemics.
Major Supporting Studies
1. Journal of Diabetes Investigation (2020)
A meta-analysis of multiple clinical trials concluded that MSC therapy significantly reduced HbA1c and insulin requirements in diabetic patients. The therapy was safe and well tolerated.
2. Zhao et al., Tissue Engineering & Regenerative Medicine (2019)
This study found that MSCs improved beta-cell function and insulin sensitivity in patients with type 2 diabetes, supporting the use of MSCs as a regenerative therapy.
3. Phase I/II Clinical Trial (2022)
A randomized placebo-controlled trial of newly diagnosed type 1 diabetes patients showed MSC transplantation led to improved HbA1c, increased C-peptide levels, and a shift from pro-inflammatory to anti-inflammatory cytokine profiles.
4. Safety Review (2021)
A review of six clinical trials involving 262 type 2 diabetes patients showed MSC therapy is safe, with minimal side effects such as nausea or mild discomfort.
Read study
Final Thoughts
For patients struggling with blood sugar control despite conventional medication, MSC therapy offers a promising adjunct treatment. By supporting natural insulin production and improving the internal metabolic environment, MSC therapy may help reduce medication reliance and enhance long-term outcomes.
Disclaimer: MSC therapy is currently under clinical investigation and should only be considered under the guidance of a qualified medical professional.
While MSC therapy is not a cure, it offers a scientifically backed pathway toward better management of diabetes, particularly in cases where insulin production is compromised.